IVF Embryo Development: Your Day by Day Guide
Emma Ebinger explains what happens behind the scenes in our lab, from egg to embryo.
Egg Collection (Day 0)
On the day of egg collection, you will speak to the doctor, a scientist and anaesthetist prior to your procedure. They will confirm your personal details, when you took your trigger injection, and the type of insemination method the lab will be using to inseminate your eggs.
During the egg collection procedure, the doctor will drain all follicles that are safely accessible. Unfortunately, not all follicles will necessarily contain an oocyte. Whilst follicle number can be a good predictor of oocyte number, it will not be until the end of the egg collection procedure that we know the actual number of oocytes retrieved.
After your egg collection procedure, you will be notified of the total number of eggs collected before you leave Day Surgery. It is important to know that not all of these eggs will be mature. An egg is mature when it has reached a genetic stage called metaphase II, and will be ready for fertilisation. On average we expect approximately 80% of eggs collected to be mature and capable of fertilisation by a sperm.

Insemination (Day 0)
There are two insemination methods available, this is decided by your Fertility Specialist depending on your past medical history and review of your semen analysis results. Insemination occurs on the afternoon of your egg collection.
Standard insemination – this is where the semen sample is processed to recover only the motile sperm, before a known number of sperm are added to the eggs. They are incubated together overnight for the sperm to fertilise the eggs.
Intracytoplasmic Sperm Injection (ICSI) – A technique where a single carefully selected sperm is injected into a mature egg. This method is usually used in cases where male infertility has been identified or there has previously been an issue with failed or very low fertilisation.
Fertilisation (Day 1)
Fertilisation is assessed 16-18 hours after insemination. For both standard insemination and ICSI methods, the scientists expect on average >70% of mature eggs to fertilise normally. You will be updated on the number of fertilised eggs on the morning of day one by either a scientist or nurse.
In approximately 5% of patients there may be failed fertilisation, where none of the collected eggs fertilise normally. This may be due to egg related factors such as immaturity or sperm related factors where the sperm have failed to bind to the egg or failed to release the male DNA to combine with the female DNA. Often there is no obvious reason why fertilisation has not occurred, and possible explanations are at a genetic or molecular level which cannot visualised or tested for.
Embryo development and Grading
At Adora Fertility, we plan for embryo transfer to occur on day 5 for most patients. In some cases, a day 3 embryo transfer may be recommended. In either case, once the eggs have been checked for fertilisation, they are assessed again on the day of your embryo transfer. We do not assess the embryos daily as this disruption can cause changes to temperature and pH of the media that the embryos are growing in and may adversely affect their development.
Prior to your embryo transfer, the embryos will be assessed to determine that they have reached the ideal developmental milestones. For day 3, this will require the embryos to have divided to between 6-10 cells. For day 5, the embryo will ideally have reached the blastocyst stage. If the embryos have failed to reach these milestones, then they are determined non-viable, and have stopped developing at an earlier stage. On average, approximately 40% of fertilised eggs will reach the blastocyst stage.
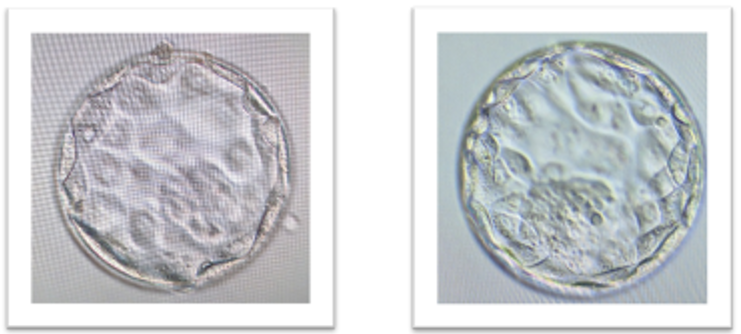
In order to determine which embryo is transferred blastocysts are graded depending on the quality and number of cells present in the embryo. Embryos are graded between 1-3, with ‘1’ being the best quality. A blastocyst has two distinct cell types:
1) the inner cell mass which forms the baby
2) the trophectoderm which forms the placenta
Both of these cell types are graded independently of one another. We classify anything with grades 1 or 2 as good quality and suitable for transfer or freezing. Embryos graded as ‘3’ are borderline/poor quality. Embryos graded with a 3 for trophectoderm can be frozen if we consider them to be borderline, and the inner cell mass is graded as good quality. We don’t freeze anything that scores a 3 for the inner cell mass. On the day of transfer, the best quality embryo will be transferred, and any remaining suitable embryos will be frozen. When it comes time to use your frozen embryos, the embryos with the highest grade will be thawed first.
Although it may be difficult, try not to put too much focus on the grades of your embryos. All embryos we transfer have a chance to result in a pregnancy and the scientists are highly trained to select the best embryo for your treatment.
Embryo Transfer (Days 3 or 5)
At Adora we aim for day 5 embryo transfer. This date and time will be confirmed by the nursing staff. The Adora embryologists will discuss your embryo development with you at your embryo transfer appointment. A picture of your best selected embryo for transfer will be displayed on the screen.
The embryo transfer is a very simple procedure, similar to a pap smear, and is performed while you’re awake. In the majority of patients there is no anaesthetic needed for this procedure.
Embryo Freezing (Days 5 or 6)
Any excess good/borderline quality embryos can be frozen for future use. Embryos are cultured in the lab until day 6, and blastocysts suitable for freezing can be frozen on either day 5 or day 6. These frozen embryos can be used at a later date in a frozen embryo transfer (FET) cycle.
Embryo freezing (a process known as vitrification) is a very successful procedure with an approximately 97% embryo survival rate. There is a very small chance that your embryo may not survive the freeze/thaw process, and if this occurs you will be notified by the scientific staff.

Freeze All Cycles
In some cases, it might be necessary to have a “freeze all cycle”. In this situation you will not have an embryo transfer and instead all suitable blastocysts will be frozen on days 5 or 6 for future treatment. Again, it is important to remember that on average we expect 40% of fertilised eggs to form a blastocyst. It is possible that not all embryos will be suitable for freezing, so a “freeze all cycle” does not mean that all embryos will be frozen, rather all suitable embryos will be frozen. In a “freeze all cycle”, the embryologists will give you a final embryology update on day 6.

Emma Ebinger is the current Scientific Director for Adora Fertility, managing the scientific operations across 4 clinics nationally. Emma started her career at Kings College Hospital, Assisted Conception Unit in London over 30 years ago and has worked in the field of embryology ever since.
Emma is passionate about delivering a high level of scientific care to patients through continuous improvements in the laboratory. Emma has been a guest lecturer for the Clinical Embryology course at USQ for many years where she shares her knowledge with the embryologists of the future.