
Starting a family can be an exciting time, however, it doesn’t always go to plan. In Australia, one in six couples experience difficulty falling pregnant at some stage in their family planning journey. Infertility can affect anyone. Overall, one-third of infertility cases are caused by female reproductive issues, one-third by male reproductive issues and the other third by combined or unknown factors.
It can be hard to know when to seek help with your family planning journey. If you are aged 35 years or over and have been trying to conceive for six months or more or are under 35 and have been trying for 12 months or more, without success, then it may be time to seek help. Assisted reproductive technologies (ART) such as in-vitro fertilisation (IVF) have been helping people to have babies since the 1970s.
Infertility Causes
Age is one of the biggest factors affecting your ability to conceive. Women are their most fertile in their 20s. Eqq quality starts to decline at 35 years of age, over 38 years of age the chances of conceiving naturally are low and over 40 the chances are very low. For males, age can also have an impact on fertility although it is not as marked as it is for women. Male sperm quality starts to decline at age 40 and there is a slight increase in some genetic conditions in the offspring of males aged over 50.
At Adora Fertility, we offer a range of fertility treatment options and treat many pre-existing conditions that can affect fertility. Some of the more common pre-existing conditions are listed below.
Female Infertility
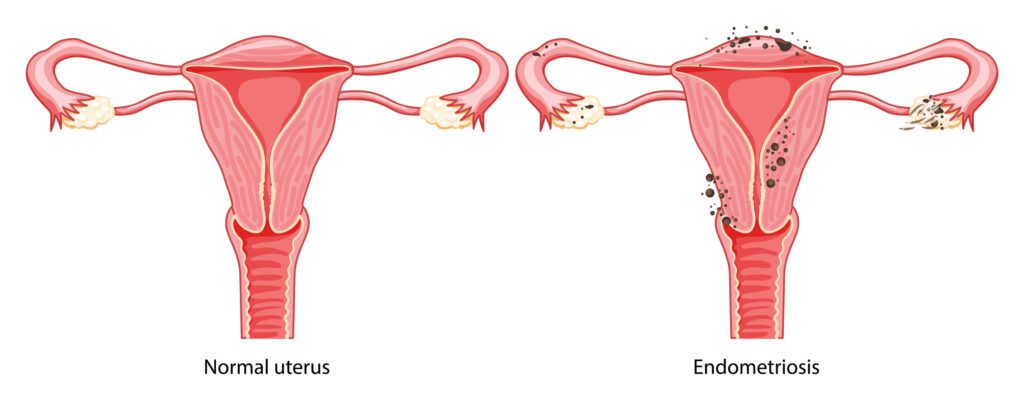
Endometriosis is a disease where tissue similar to the lining of the uterus, the endometrium, grows outside of the uterine cavity. Abnormal places where this tissue can grow include on the ovaries, tubes, bowel, the lining that covers the pelvis and, in more rare cases, other parts of the body including the bladder and lungs.
The tissue that grows outside of the uterine cavity behaves very similar to the uterine lining and is responsive to the hormonal changes that happen with a menstrual cycle. As a result, the tissue grows and breaks down like the uterine lining does. Whilst within the uterus the products of the lining breakdown come away as menstrual blood, the tissue that breaks down outside the uterus becomes trapped within the pelvis.
This continued process of growth and breakdown eventually causes scar tissue to form and can cause adhesions over time. This can lead to severe pain and cramping, inflammation and abnormal or heavy periods. There can also be anatomical distortion that can impair the egg and sperm from meeting or transportation of the embryo down the tube. The inflammation may decrease the egg quality and harm implantation.
Polycystic Ovarian Syndrome (PCOS) is a hormonal condition where women may experience irregular menstrual cycles, excess body hair and acne. The exact cause of PCOS is not known. Studies point to lifestyle, environment and genetics as the key factors. High body weight, high carbohydrate or a fatty diet and lack of exercise are strongly associated with the rise in incidence of PCOS.
It has been shown that up to 80% of women with PCOS are ‘insulin resistant’ which means that their bodies don’t recognize the insulin levels produced in response to the intake of carbohydrates and therefore continue to produce insulin resulting in an excess. Hormonal imbalances cause the body to produce more androgens (male sex hormones). There is dysregulation of the brain to the ovarian hormonal axis which disrupts ovulation and the menstrual cycle which can make it more challenging to fall pregnant.
Despite its name, PCOS affects the whole body, not just the ovaries. Uncontrolled PCOS can lead to an increased risk of diabetes, hypertension, increased cholesterol levels and heart disease.
Fibroids are common, non-cancerous growths of muscle which form in the muscle wall of the uterus. Fibroids can vary in size, ranging from the size of a pea to the size of a melon or larger and they don’t always cause symptoms or need treatment. Fibroids are also called uterine fibromyomas, leiomyomas or myomas and may grow in different layers of the uterus. It’s not entirely clear what causes fibroids to develop, however, it is thought that the female hormones oestrogen and progesterone stimulate the growth of fibroids.
Symptoms of fibroids can include heavy or long periods, painful periods, bleeding in between periods, iron deficiency, pain during intercourse, a feeling of heaviness in the back, bowel or bladder and the need to urinate frequently. If fibroids are very large or affect the uterine cavity they can cause difficulties with a pregnancy implanting or lead to miscarriage.
The fallopian tubes are a pair of thin tubes, one on each side of the uterus. It is within the tube that the egg is fertilised by the sperm and the tube then facilitates the transport of the dividing embryo to the uterus. Fallopian tubes can become blocked or damaged. This is most commonly caused by pelvic inflammatory disease (PID), an STD infection namely chlamydia or gonorrhoea or a uterine infection usually associated with abortion, miscarriage or pelvic surgery. Endometriosis and fibroids are also associated with blockages.
Similar to many other causes of infertility, woman may not necessarily experience any symptoms. For those that do experience symptoms they can include abdominal pain, fever, painful periods, malodorous vaginal discharge or pain associated with urinating or intercourse.
Recurrent miscarriage is when a couple has lost three or (in some guidelines) two pregnancies prior to 20 weeks. Recurrent miscarriages are both devastating and disheartening for the couple and the treating specialist. A single miscarriage is quite common (around 1 in 5 pregnancies depending on age) however, recurrent miscarriage is much more uncommon. Even when a number of tests are conducted, frustratingly a cause is found in less than 50% of couples. The commonest cause of miscarriage is an abnormal chromosome number in the baby. As chromosome abnormalities in the egg increase with age, miscarriage also increases with age.
If you suffer from recurrent miscarriage, potential causes that will be investigated include genetic or chromosome problems in both the female and male, uterine abnormalities, general health problems such as thyroid disease, hyperprolactinemia, PCOS, diabetes and coeliac disease. Antiphospholipid Syndrome is a known cause of recurrent miscarriage. Certain blood clotting disorders, known as thrombophilias, may have an association with recurrent miscarriage but the evidence is not clear.
Secondary infertility occurs when you can’t become pregnant for a second time. If you have had a baby previously, it may come as a shock to learn that you have trouble on your second or subsequent attempts at conception. The chances of secondary infertility are more common than you might think. Unfortunately having one child is no guarantee that you can easily conceive a second or subsequent time.
Causes of secondary infertility are not dissimilar to the causes of those experiencing primary fertility (difficulties conceiving first time around). The most common reason couples experience secondary infertility is that they are older when they are trying to conceive their second child and therefore the egg quality is lower.
Male Infertility
Male infertility is any health issue in a male that lowers the chances of his ability to conceive. The most common causes of male infertility are usually related to the production of sperm, namely poor quality sperm, low sperm count or blockages in the tubes of the reproductive system. Damage to the testicles due to an injury or illness, ejaculation disorders and lifestyle factors are also common causes of infertility in males.
There are many reasons for infertility and just because you have one of the conditions listed here, it doesn’t mean you are infertile or unable to conceive.





The impact of lifestyle on fertility
There are a number of lifestyle factors that can have an impact on your fertility. Maximising your health and wellbeing is the first step to improving your overall chance of pregnancy. For both males and females, simple lifestyle changes shouldn’t be overlooked when it comes to improving your fertility and chance of conceiving.
Diet
A well balanced diet is important. The Mediterranean type diet has been shown to be potentially good for fertility. Meals that include an adequate intake of good fats, fish, iron and fruits and vegetables are an excellent start. Diets that are high in saturated fats, simple sugars or alcohol can lead to reduced fertility in both males and females. In addition to a healthy diet, there are some vitamins and minerals that could give your fertility a boost. These include folic acid, anti-oxidants, vitamin B12 and omega- 3 fatty acids. Folic acid and iodine are recommended for woman planning a pregnancy and throughout their pregnancy for proper development of their baby.
Weight
Weight is an important consideration. Women who are overweight or underweight can face difficulties conceiving as weight can affect your ovulatory cycle. Being overweight may also increase the risk of miscarriage or increase the risk of obstetric complications. In men, obesity can lower sperm count by up to 50%. Overweight men are also more likely to suffer erectile dysfunction and have a higher rate of DNA fragmentation in sperm. Moderate exercise has clear benefits for health and wellbeing and can also have a positive impact on fertility.
To determine if you are within a healthy weight range, we use your Body Mass Index or BMI. Use our BMI calculator to determine your BMI.
BMI Calculator
To understand the meaning of your BMI result, we recommend visiting the Australian Government Department of Health website.
Smoking, Alcohol & Recreational Drugs
Smoking is toxic to the health of eggs and sperm and will lower the chance of conception. The best advice when it comes to smoking/vaping and other recreational drugs is to cut it out completely. Couples should minimise their alcohol intake to a very safe level or avoid altogether and restrict their caffeine consumption to one normal coffee or equivalent per day.
Every individual and couple are unique and every scenario is different. Sometimes, even with the healthiest of lifestyles and no pre-existing conditions, conception still proves difficult (known as unexplained infertility).
Maximising your health and wellbeing is the first step to improving your overall chance of pregnancy.
Assessing your fertility
At Adora Fertility, a fertility assessment is the first step towards understanding your fertility health. We will recommend the tests you should undertake and these tests can be arranged through an Adora Fertility GP or your own GP who will also be able to recommend the most appropriate pathology clinics for you to complete your fertility tests. For rural patients we can recommend pathology clinics nearest to you. For males, there is the option to undertake the semen analysis in the comfort of your own home. The semen analysis is the most comprehensive test for understanding male fertility. We recommend Sapyen, supplier of the world’s first complete at home sperm health and fertility test.
The most common tests for understanding your fertility are outlined below.
For Females
For Males
Results from your fertility assessment provide a comprehensive understanding of your fertility health and will assist your Fertility Specialist with formulating your individualised treatment plan.
