How embryos are graded
Ever wondered how Embryologists grade embryo’s? What determines the stage of embryo development and the quality of each embryo? One of our Adora Embryologists, Jaime Wheeler, explains.
Following the fertilisation check that occurs the morning after an egg collection, the embryos are left undisturbed until the morning of the embryo transfer or embryo freeze. At this time, the Embryologist will assess each embryo under high power magnification and record the developmental stage, and quality of each.
There are many grading systems which exist, and the way an embryo grade is reported will vary between IVF clinics. It’s important to know that while the format of the grade may be different depending on the system used, they all work to convey the same information about embryo development and quality.
At Adora, most embryo transfers occur on Day 5 of development. In some cases, as decided by the treating specialist, an embryo transfer may be scheduled for Day 2 or 3. Due to the different developmental characteristics of Day 2/3 (cleavage stage) embryos and Day 5 (blastocyst stage) embryos, two separate grading systems are used.
Cleavage Stage Grading (Day 2/3)
For Day 2/3 transfers, an embryo is expected to have between 2-6 cells (day 2), and 6-10 cells (day 3). The Embryologist is highly trained to count the individual cells within a cleavage stage embryo and observe any existing fragmentation. Fragments refer to small blebs of the inside of the cell that break off and become excluded from the embryo during cell division. Some degree of fragmentation is considered normal however high degrees of fragmentation may indicate poor cell integrity and these embryos have reduced potential to reach the blastocyst stage.
Cleavage stage embryo grades consist of the number of cells in the embryo, followed by a single numerical grade which encompasses the degree of visible fragmentation and cell symmetry. The grade ranges from 1-3, where grade 1 and 2 embryos are considered suitable for transfer, while grade 3 embryos are poorer in quality and would not be selected for transfer on Day 2/3. Embryos not transferred on Day 2/3 will be cultured (grown) to Day 5 and reassessed to determine whether they were able to reach the blastocyst stage.
Below is a summary of the cleavage stage grading criteria used by Embryologists at Adora, with an example of what each embryo grade may look like down the microscope.
| Grade | Description |
| 1 | Embryos that have reached the appropriate stage of development with no or minimal (<10%) fragmentation |
| 2 | Embryos that have reached the appropriate stage of development but have moderate (10-25%) fragmentation. |
| 3 | Embryos that have significantly delayed growth, significant fragmentation (>25%) |
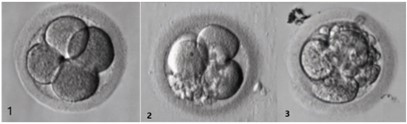
Example: An embryo which has 4 cells, minimal fragmentation, and even cell division would be assigned the grade 4C1.
Blastocyst Stage Grading (Day 5/6)
By day 5, good quality embryos should have reached the blastocyst stage of development. Unlike cleavage stage embryos, blastocysts have hundreds of cells and a distinct fluid filled cavity.
Blastocysts are assigned an alphanumeric grade. The letters describe the stage of blastocyst development. The numbers describe the quality of the two distinct cell types within the embryo, and range from 1 (excellent) – 3 (poor).
Example: XB1/2. An embryo that has reached an expanded blastocyst (XB) stage with an excellent quality inner cell mass (1), and an acceptable trophectoderm (2). Overall grade: XB2.
Let’s take a closer look…
What are the stages of blastocyst development?
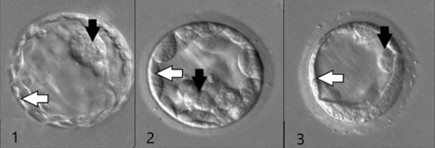
Embryos move through various stages of blastocyst development as they gain more and more cells over time. The degree of expansion of a blastocyst is dictated by the size of its cavity and the number of cells present. The image below shows (1) a very early blastocyst VEB, (2) an early blastocyst EB, (3) a blastocyst B, (4) an expanded blastocyst XB, and (5) a hatching blastocyst HB.
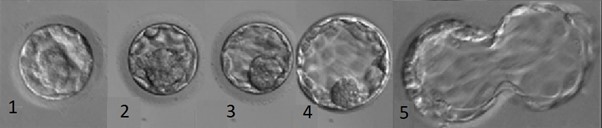
Eventually, all embryos resulting in pregnancy will pass through each of these stages before implanting into the wall of the uterus. An embryo will be considered for transfer if it has achieved any degree of blastocyst formation.
How are the cells of a blastocyst graded?
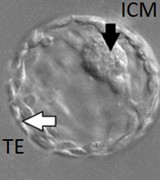
There are two different types of cells within a blastocyst; those that make up the inner cell mass (ICM) which ultimately becomes the fetus, and the outer ring of trophectoderm cells (TE) which forms the placenta. Both cell groups are equally important and are each graded independently based on their quality.
Embryos are suitable for freeze or transfer when they receive a grade 1 or 2 for the ICM alongside a grade 1, 2 or 3 for the trophectoderm. On occasion, as decided by the embryologist and specialist, embryos graded with an ICM of 3 may still be considered for a fresh embryo transfer. While they have been shown to have a reduced chance of success, there are still healthy babies born from poorer grade embryos.
Below is a summary of the criteria used by Adora Embryologists to grade the cells of the ICM and trophectoderm, with an example below of what a grade 1, 2, and 3 embryo may look like down the microscope.
Describing the Inner Cell Mass ICM (black arrows below)
| Grade | Rating | Description |
| 1 | Good | Prominent, easily discernible, with many tightly packed cells |
| 2 | Fair | Easily discernible, with many cells loosely grouped together |
| 3 | Poor | Difficult to discern, few cells, or loosely grouped |
Describing the Trophectoderm TE (white arrows below)
| Grade | Rating | Description |
| 1 | Good | Many cells forming a cohesive, even layer of cells |
| 2 | Fair | Fewer cells forming a loose or inconsistent layer of cells |
| 3 | Poor | Very few cells, significant granularity or significant unevenness |
How important is the grade of an embryo?
The grade of an embryo works to summarise its ‘appearance’ which helps inform clinical and laboratory decisions including which embryo to select for transfer, which day the transfer should take place, and if it is appropriate to consider a double embryo transfer. While embryo grades are a useful tool, they only make up part of the picture. Clinical decisions will also consider personal medical history, patient age, previous IVF cycle outcomes, and the number of embryos available within each cycle.
While there are criteria to assist the Embryologist in assigning a grade, ultimately embryo grading is a subjective process. It is also important to remember that there are other factors of embryo quality that cannot be seen down a microscope, such as what is happening within the cells of the embryo on a genetic level. These reasons help explain why some embryos with a seemingly perfect grade may not lead to pregnancy, while some with poorer grades still do.
It is important to remember that pregnancies can result from embryos of all grades, at any stage of development. If the transfer of the ‘best’ available embryo does not result in a pregnancy, it is not to say that there won’t be success with other embryos that may have been assigned a lower grade. Each embryo that has met the criteria for transfer or freezing has a unique potential to create a perfectly healthy baby.
References
Balaban, B., Urman, B., Sertac, A., Alatas, C., Aksoy, S., & Mercan, R. (2000). Blastocyst quality affects the success of blastocyst-stage embryo transfer. Fertility and Sterility, 74(2), 282-287.
Cimadomo D, Sosa Fernandez L, Soscia D, Fabozzi G, Benini F, Cesana A, Dal Canto MB, Maggiulli R, Muzzì S, Scarica C, Rienzi L, De Santis L. (2022) Inter-centre reliability in embryo grading across several IVF clinics is limited: implications for embryo selection. Reprod Biomed Online. Jan;44(1):39-48. doi: 10.1016/j.rbmo.2021.09.022.
Education zone /Fertilitypedia. Available at: https://fertilitypedia.org/edu (Accessed: 28 June 2023).
Honnma, H., Baba, T., Sasaki, M., Hashiba, Y., Ohno, H., Fukunaga, T., … & Asada, Y. (2012). Trophectoderm morphology significantly affects the rates of ongoing pregnancy and miscarriage in frozen-thawed single-blastocyst transfer cycle in vitro fertilization. Fertility and sterility, 98(2), 361-367.
R, Hurtado & R, de & Valle, Mariela & Sampaio, Marcos & Geber, Selmo. (2021). In vitro Human Embryo Morphology – An Odissey Outside the Oviduct. Austin Journal of Anatomy. 8. 10.26420/austinjanat.2021.1099.
Thompson, S. M., Onwubalili, N., Brown, K., Jindal, S. K., & McGovern, P. G. (2013). Blastocyst expansion score and trophectoderm morphology strongly predict successful clinical pregnancy and live birth following elective single embryo blastocyst transfer (eSET): a national study. Journal of assisted reproduction and genetics, 30, 1577-1581.