Endometriosis and the impact on fertility

Endometriosis is a painful condition affecting around 1 in 9 women in Australia. Although it can be harder to fall pregnant if you suffer from endometriosis, most women are still able to have children and many become pregnant without any medical intervention. In this blog, Dr Maha Ragunath, Fertility Specialist at Adora Fertility Perth, discusses endometriosis, the symptoms and treatments and what to do if you suspect you might have this condition.
What is Endometriosis?
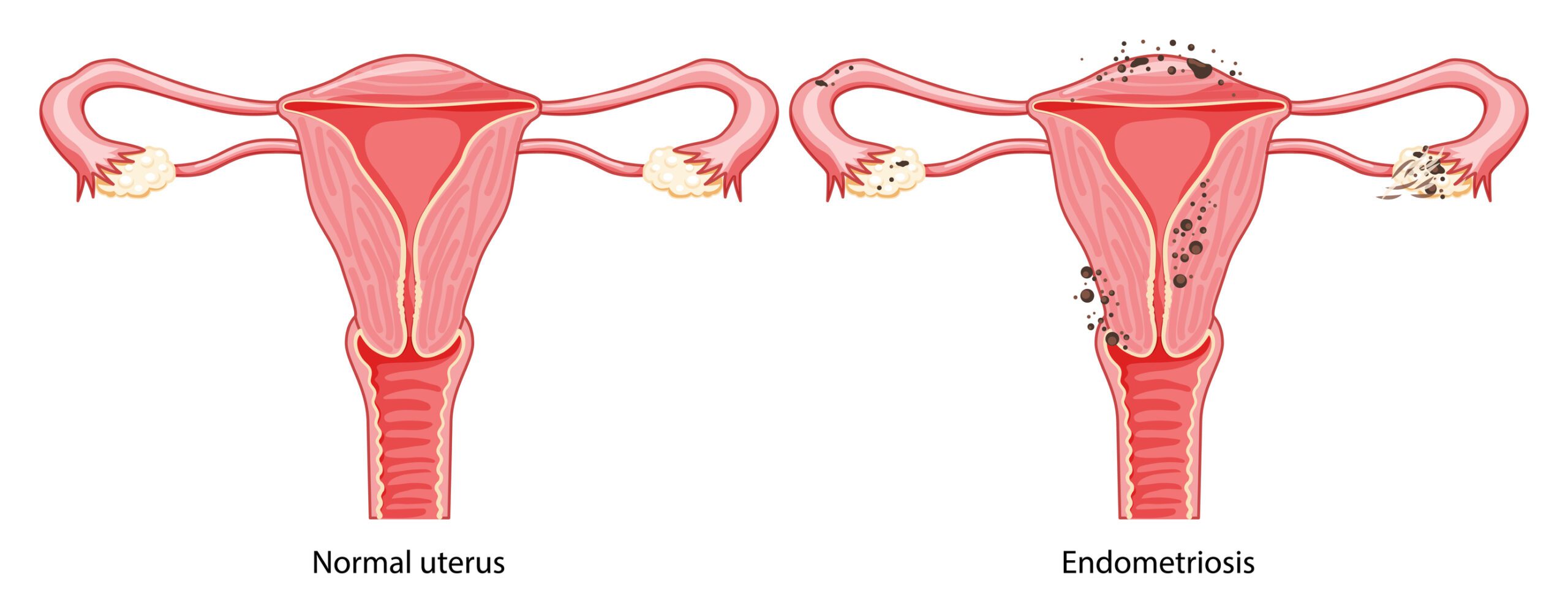
Endometriosis is a disease where tissue, similar to the lining of the uterus, grows outside the uterine cavity. Abnormal places where this tissue can grow include on the ovaries, tubes, bowel, the lining that covers the pelvis and, in more rare cases, other parts of the body including the bladder and lungs.
The tissue that grows outside the uterine cavity behaves very similar to the uterine lining and is responsive to the hormonal changes that happen with a menstrual cycle. As a result, the tissue grows and breaks down like the uterine lining does. Whilst within the uterus the products of the lining breakdown come away as menstrual blood, the tissue that breaks down outside the uterus becomes trapped within the pelvis. This continued process of growth and breakdown eventually causes scar tissue to form and can cause adhesions over time. This can lead to severe pain and cramping, inflammation, abnormal or heavy periods and can make it harder to fall pregnant.
Endometriosis is a progressive and chronic condition, meaning it generally gets worse over time. Endometriosis can start with your first menstrual period and last until menopause. It is a common disease that affects approximately 10% of women worldwide. Around 1 in 9 women in Australia are diagnosed with endometriosis – with an incidence of 30 – 50% of endometriosis in women who are infertile.
Stages of Endometriosis
Endometriosis is staged from minimal to severe which reflects the extent of the disease rather than the severity of symptoms. Each stag is characterised by the number, depth, and location of endometrial impants, as well as the presentation and severity of adhesions and endometriomas (cysts). A points system is used to provide a standardised and measurable way to assess the severity and extent of the disease. This points system will help your Fertility Specialist or treating healthcare professional to predict potential fertility outcomes and guide treatment decisions. The stages of endometriosis are outlined below.
Stage I (1-5 points)
- Minimal
- Few superficial implants
Stage II (6-15 points)
- Mild
- More and deeper implants
Stage III (16-40 points)
- Moderate
- Many deep implants
- Small cysts on one or both ovaries
- Presence of filmy adhesions
Stage IV (>40 points)
- Severe
- Many deep implants
- Large cysts on one or both ovaries
- Many dense adhesions
What are the Symptoms of Endometriosis?
Women can present with varying symptoms depending on where the abnormal tissue is located. The most common symptoms of endometriosis include:
- Menstrual cramps and heavy periods, with pain typically rising to a peak just prior to the onset of a period and being relieved by the flow
- Pain during intercourse
- Pain with bowel movements or urination
- Heavy periods, sometimes with premenstrual spotting
- Lower back pain
- Infertility
The seriousness of your pain is not necessarily a sign of the number or extent of endometriosis growing in your body. You could have a small area affected with excessive pain or a large area affected with little or no pain.
It can take some time to get a diagnosis of endometriosis because symptoms vary between women and change over time. In addition, period pain is often accepted as normal. A thorough review of your symptoms, medical history and test results will improve your chances of an early diagnosis.
Endometriosis and Infertility
The relationship between endometriosis and infertility has been debated for years. Endometriosis can reduce fertility, with 30-50% of women affected by endometriosis experiencing infertility.
When abnormal tissue grows around or on the ovaries or tubes this can cause inflammation with subsequent scarring which can then, in turn, cause obstruction to tubes and reduce egg reserves (or reproductive potential) on ovaries. Sometimes endometriosis can grow within the muscle of the womb – a condition called Adenomyosis which can impact embryo implantation. Endometriosis has also been shown to alter the immune system and change the hormonal environment around the eggs, which can impair egg quality.
Certain endocrine and ovulatory disorders including luteinised unruptured follicle syndrome (LUFS), impaired follicular development, luteal phase defects and premature or multiple luteinising hormone surges can all be associated with the condition. These are generally treatable with the right advice and medications.
Treatments for Endometriosis
There are several medical and surgical options available to help reduce the symptoms of endometriosis. It is usually recommended, initially, to try conservative treatments such as pain and hormonal medications to help control growth and reduce pain.
Sometimes the use of hormonal contraception like combined pills and depot provera injections will be recommended to keep symptoms at bay. Hormone medications such as GnRH agonists and antagonists, which block the production of oestrogen by the ovaries, can sometimes be used as a temporary measure as they prevent menstruation by creating an environment of artificial menopause. Some patients may need to add back hormone therapy to prevent hot flushes and vaginal dryness, which can be debilitating. These options are not suitable for women trying to get pregnant and are usually short term solutions as they can cause side effects such as weight gain, reduction in bone thickness and depression.
For women planning on having a family, surgery is usually the best option. Laparoscopy or keyhole surgery is used to visualise and diagnose endometriosis and can be used to remove or destroy abnormal and excessive endometriotic deposits. Surgery can also improve natural conception rates and is the recommended treatment for mild endometriosis.
For those with moderate to severe endometriosis, it is not clear whether surgery will actually improve the success rate for IVF. Sometimes aggressive surgical treatment of endometriosis as in excision of endometriosis from the lining of the pelvis (peritoneum) or removing cysts from the ovaries can be counterproductive by reducing blood flow and diminishing egg reserves.
Not all endometriosis will need treatment. Treatment of endometriosis is recommended to treat symptoms (mostly pain), infertility or when your quality of life has suffered. Sometimes people find their symptoms worsen with treatment.

Next Steps
There are a number of different options for those with endometriosis and due to the complexity of the condition, the treatment plan can be wide and varied. If you are trying to fall pregnant, it is best to see a Fertility Specialist, who can guide you on the most appropriate treatment or combination of treatments for your needs.
A Fertility Specialist will conduct a careful clinical assessment of your symptoms, aided by imaging such as a pelvic ultrasound or an MRI. This can provide a clearer picture of the grade or severity of the condition, which will help guide treatment. A Fertility Specialist will also help guide the timing of treatments and potential surgery so that outcomes, and your chances of falling pregnant, are optimised for you.
At Adora Fertility, our Fertility Specialists would welcome the opportunity to discuss your situation with you. Please contact us to find out how we can help.



