
Success rates are one of the many ways you can compare fertility providers and often form part of the decision-making process when it comes to choosing a fertility clinic. At Adora, we are both transparent and proud of our success rates, we work hard to maintain success and are continuously striving to improve outcomes for our patients.
We hope the information provided here will help you understand and interpret success rates, recognise their limitations and know where to look for comparative data. Our aim is to provide you with as much information as possible so you can make an informed decision.
Understanding success rates
While IVF success rates can be presented in many different ways, the data most commonly used to report the success of IVF treatment cycles is the number of clinical pregnancies and live births that result. Although this sounds relatively straightforward, IVF is a complex field of medicine and comparing success rates can also be complex as there are a number of factors that can affect results. In addition, it is important to note that not every treatment cycle will result in an egg collection, an embryo transfer or embryos available for freezing.
Age, weight, lifestyle choices and the specific cause of infertility are just some of the factors contributing to the likelihood of achieving a pregnancy and live birth for each patient. Age is one of the most significant factors impacting success with advanced age in the female associated with a decrease in clinical pregnancies and live births. Being underweight or overweight can also impact clinical pregnancies and live births, as can certain lifestyle factors such as smoking. There are a large number of lifestyle factors and infertility causes which all have varying impacts on the success of fertility treatment.
Not only does each patient bring their own set of circumstances, but each clinic can vary in their approach. Clinics that are open to helping as many people as possible, or that see difficult cases that have been unsuccessful elsewhere, may see a reduction in success rates. Age cut-off and BMI (indicating body size) cut-off can differ between clinics and these are all important differentiators which impact success rates.
It is very difficult to compare clinic success rates fairly as they are largely dependent on the types of patients a clinic treats and no two patient populations will be the same.
While success rates are an important consideration, they should not be the only consideration when choosing a fertility clinic. We would recommend looking at the clinic as a whole and considering things like the qualifications of the specialists, the costs, whether the clinic is easily accessible, the quality of care and the range of services provided.

Our success rates
Our success rates are proof that high quality fertility treatments can be delivered at an affordable cost. These graphs show our success rates for 2023 (the most recent data available) averaged across all Adora Fertility clinics. The data shown here includes all IVF treatment cycles where patients underwent an embryo transfer as part of an IVF or ICSI treatment cycle. The first graph includes data for fresh cycles (where an embryo is transferred at the time it is created) and the second graph includes data for frozen cycles (where the embryo has been stored and transferred at a later date).
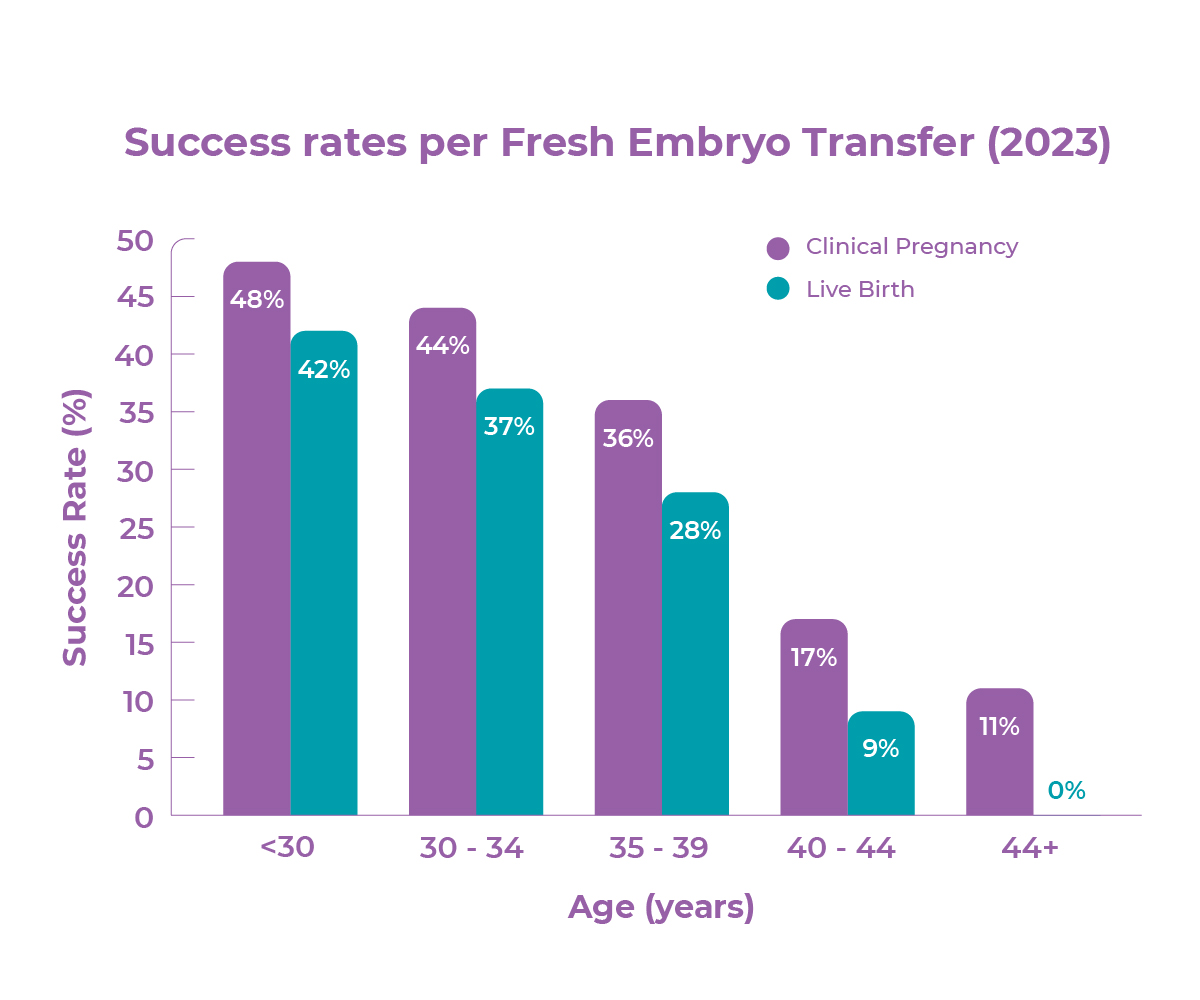
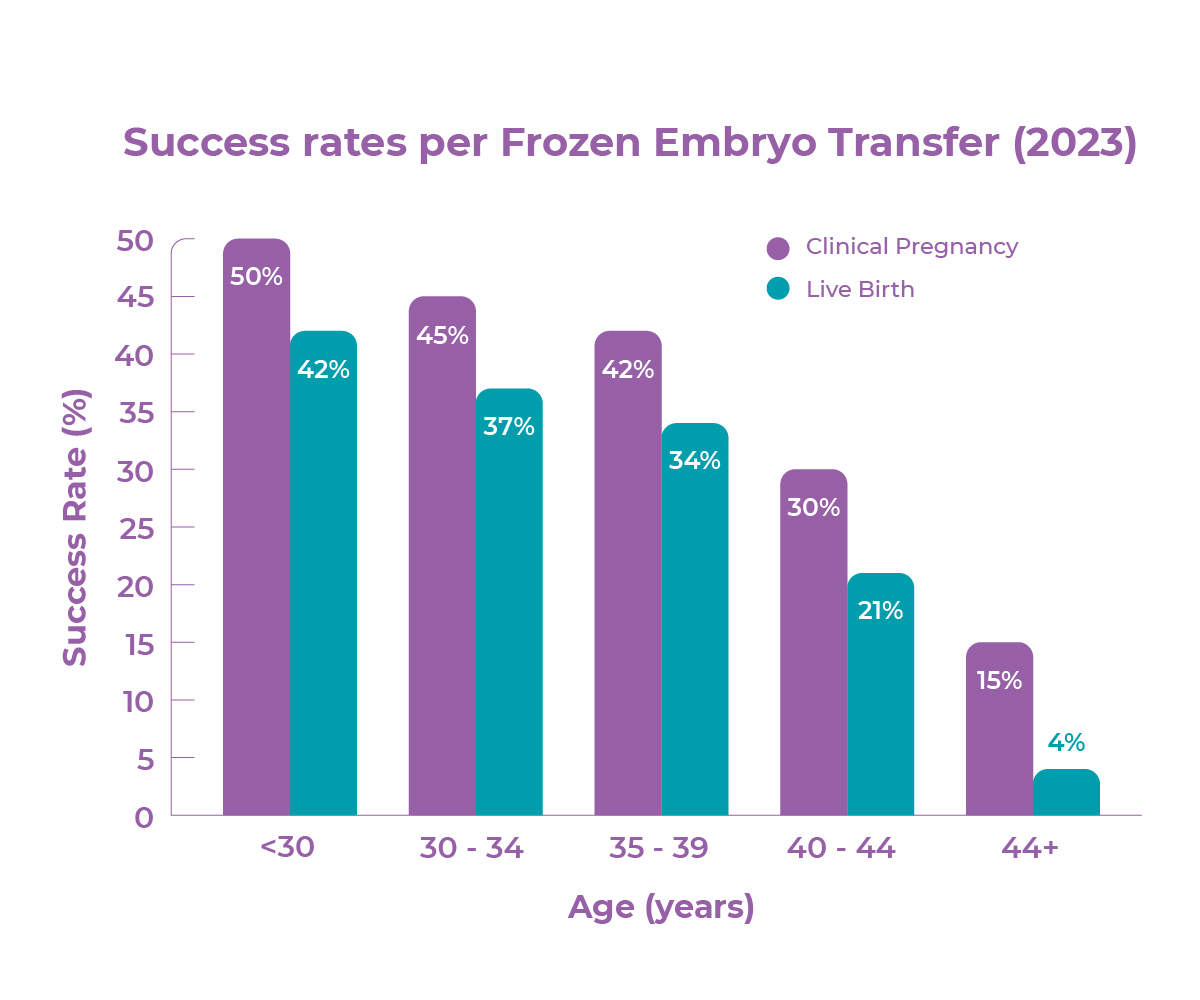
To understand our success rates in a little more detail it is worth making note of two important points. The first point relates to the use of donor eggs and sperm. No donor cycles are included in our data. For clinics that do include donor cycles, success rates are likely to be higher. This is because donor cycles are usually for women who do not have an underlying fertility issue (ie. single woman and same sex couples).
The second point relates to preimplantation genetic testing (PGT) of embryos and is a little more complex. No PGT embryos are included in our data. For clinics that report on all cycles involving an embryo transfer, as we have done, and uses PGT embryos then success rates are likely to be higher as the embryo has survived the testing process prior to embryo transfer. If, however, a clinic reports on all cycles regardless of whether an embryo transfer took place or not, and uses PGT embryos then success rates are likely to be lower as PGT can harm embryos. Adora Fertility has chosen not to undertake genetic testing of embryos for their chromosome status (PGT-A), because it is not covered by Medicare and has not been convincingly shown to increase pregnancy rates overall.
We are proud of our success rates which are proof that success can be achieved at an affordable cost.
Your IVF success website
The YourIVSuccess website, created and funded by the Australian Government, in partnership with University of New South Wales, provides an independent source of IVF success rates for accredited IVF clinics across Australia. You can view IVF clinic success rates all in one place along with information about each clinic.
When comparing clinics through this website it is important to note that there will be differences in both the patient cohort, the way a clinic approaches IVF treatment and the ways that success rates are calculated across clinics. Some clinics include donor cycles and PGT embryos and some don’t.
Within the YourIVFSuccess website there is an IVF success estimator tool which estimates your chance of having a baby through IVF based on the data you input. It is important to remember that this tool should not replace the advice of your Fertility Specialist who will be able to give you the most accurate chance of success based on your specific situation. As we have said before, it is really important that these measures are used as a guide only. If you would like some further assistance with understanding success rates, please do contact us.
Book your first bulk-billed consultation with us today!

